Feeling Overwhelmed? Managing Academic Pressure
Exams are coming up. You have assignments and projects due in all your classes. You are scheduled to work. Your family has expectations of you, and you have expectations of yourself. Academic pressure, along with other responsibilities, can be a lot for students.
What is academic pressure?
Academic pressure can be defined as a fear of failure, having concerns about the future, chronic stress about workload and exams, worries about parental expectations, and competition with peers for grades.[1]
The weight of academic pressure can affect students’ mental health and show up differently.
Students can find themselves dealing with:
- anxiety over an assignment they do not understand
- sleeplessness from long hours of studying for an exam
- loneliness from being away from family and friends
- low mood from not having time to participate in social activities
- lack of appetite or overeating to cope with a stressful schedule and semester
It is a lot dealing with these feelings both at home and at school, and the pressure can sometimes feel like too much to manage.
How to manage academic stress
We cannot live in a completely stress-free world, but not all stress is bad.
The Yerkes-Dodson model says that having some stress can actually help us achieve our goals. For example, stress about an essay due in two days might motivate a student to sit down and knock it out. Having several deadlines at the same time can motivate another student to prioritize what needs to be completed first. These are positive ways that stress can work in our favour.
However, at too high a level, stress can become a problem. When stress is too high, it can be felt constantly and may interfere with mood and day-to-day life. This can show up in not wanting to get out of bed for several days, skipping meals or avoiding things that once brought you joy.
If academic pressure and stress are feeling like a lot, here are some tips that may help:
- Realistic time management. Sometimes the thing that makes us the most stressed is that we have not allotted enough time to complete what we must do, and it catches us by surprise. For example, you might think that you can get through your assigned reading in an hour, but it might actually take you three hours. If you have not allotted enough time for this, you will always feel behind. Many post-secondary institutions have resources that can help you manage your time.
- Learning to say no. This is a tough one but learning how to say ‘no’ can alleviate stress and burnout. We can’t always do everything and achieve our goals. You may need to cut down on extra-curricular activities or take a semester with one less course and catch up in the summer. Take some time to re-evaluate where you spend your time. Minor modifications now could mean a better handle of the academic year. Remember, school is a marathon, not a sprint. Many universities and colleges have student services and program advisors who can help you explore your options.
- Focus on the now. Take a deep breath. Focus yourself. Sometimes we can start to spiral and become anxious about all the things we need to do and the time we have to do them. Mindfulness helps us to calm our minds and be present in the moment—this allows us to focus on the right now instead of worrying about the future. Downloading apps like Calm or Headspace can help you to relax, be mindful and develop more effective ways of thinking.
- Make time for you. For many students’ their schedule is jam packed with lectures, tutorials, reading and homework. It is easy to forego relaxation or fun because there are not enough hours in the day. The thing is, we all need activities in our life that spark joy and give us time to decompress. Even if it is short 10-minute dance between readings, calling up a friend for a walk or going out to a new restaurant. By making time for these activities, we ensure we can take care of our mental health in a way that supports our energy and focus for school.
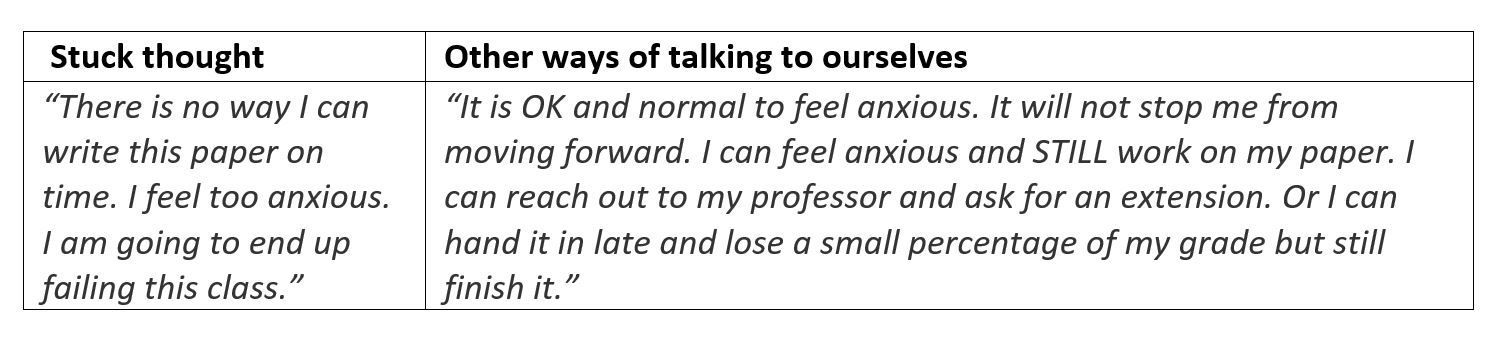
- Give yourself some grace. When you feel your mind spiraling and that negative internal voice starts to speak up, take a moment to pause. Try taking a moment to acknowledge the challenging situation you are in. Consider how you would respond to a loved one like a friend or family member in the same situation. Try to catch your unhelpful thoughts and give yourself some grace and patience. Here is an example of taking a thought that may be keeping you stuck in a negative place and channeling it into a thought that may be more helpful.
Get the support you need
If you are feeling overwhelmed by academic pressures, you can get support. Talk to a trusted friend. Visit your school’s student services or wellness department. Contact a community health organization or your family doctor.
If you are not sure where to turn but know that stress, feelings of sadness or worry are getting to be too much, you can reach out to us for support. We have trained and understanding coaches and therapists that can help you virtually, over the phone or in-person. They can even work around busy school schedules through online support, check-in calls and video conferencing. We want you to feel supported, no matter where you are.
It is hard being a student, but it can be even harder when you go at it alone.
Remember, ask for help when you need it.
References
---
The Ontario Structured Psychotherapy (OSP) program offers free, evidence-based, cognitive-behavioural therapy (CBT) to adults (18+) in Ontario who are experiencing depression or anxiety related concerns.
We listen to you and match you to the service and care that best meets your needs. Whether that’s reading materials in your own time, engaging with online tools, or speaking to us virtually, by phone or in-person – we meet you where you are.
CarePoint Health leads and coordinates access for Ontarians to the free OSP program for the regions of Brampton, Halton, Mississauga, and South Etobicoke. In collaboration with our partners, we deliver mental health services and improve access to care.














